Imagine your child’s brain as the world’s busiest train station, trains (movements) rush in and out, some right on time, others darting out when you least expect. Now, picture that one of the traffic controllers, the basal ganglia, starts letting trains go when they shouldn’t, making movements feel impossible to hold back. If you’re wrestling with your kid’s tics, you know this scenario all too well.
Here’s the truth: It’s not a matter of willpower or parenting, and it’s definitely not a sign of a broken brain. Usually, it’s a classic case of miscommunication in a brain circuit that’s working a bit too enthusiastically. Curious how? Stay with me as we pull back the curtain on the basal ganglia tic pathways (CSTC pathway) and the brain’s very own movement “gate.” We’ll use real-life analogies, parent-to-parent advice, and simple takeaways so you finally feel in-the-know, and maybe a little less alone on this bumpy ride.
Key Takeaways
-
The basal ganglia act as the brain’s movement gatekeeper, and miscommunication in these pathways leads to tics in children.
-
Tics are not caused by weak willpower or brain damage, but rather by overstimulated circuits in the CSTC pathway involving the basal ganglia.
-
Triggers like stress, fatigue, and screen time can heighten tics, while routine, sleep, and focused activities help regulate the basal ganglia pathways.
-
Balanced dopamine levels in the basal ganglia and CSTC pathway are crucial, as excess dopamine can make tics more frequent or intense.
-
Behavioral interventions like CBIT and simple lifestyle adjustments can support children with tic disorders, with medical evaluation reserved for severe or disruptive cases.
Table of Contents
The Brain’s Movement Gate: What This Article Explains
Parents often wonder, ‘Why can’t my child just stop those sudden movements or sounds, even when they’re trying their hardest?’ If you’ve heard baffling science words like “basal ganglia” or “CSTC pathway” and felt more lost than enlightened, this is the guide for you.
Here’s our promise: you’ll finish this read actually understanding how tics start inside the brain, why the signals can feel so uncontrollable, and how real neurological research (from pediatric neurology and brain imaging) finally starts making sense.
Expect plain talk, relatable stories, and plenty of myth-busting. We’ll even peek into natural remedies, lifestyle tweaks, and innovative, expert-backed ways to support your child, no medical degree required.
What Are the Basal Ganglia?
The Brain’s Motor Control Center
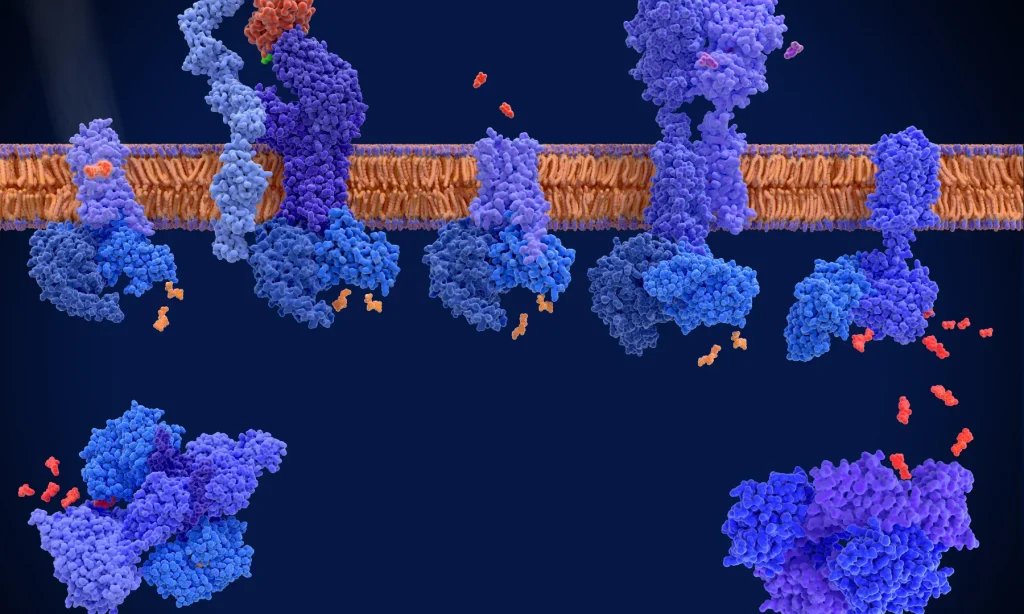
Let’s get one thing straight: the basal ganglia aren’t some mysterious, malfunctioning part of “problem brains.” They sit deep inside everyone’s head, acting as the brain’s traffic controller. Imagine someone in an air-traffic control tower, deciding which planes (movements) take off and which should hold at the gate.
For your child, these clusters help pick which movements to start, and, crucially, which ones to STOP. This control isn’t just for significant, planned actions (like walking), but also for all those tiny, everyday habits, blinking, tapping, swallowing, and yes, the startle of a sudden tic.
Key Parts (in plain English)
You don’t need neurology flashcards; here are the real stars of the show:
-
Striatum: Think of this as the “entry gate.” It decides which signals coming from the outer brain (cortex) are allowed through, for movement, emotion, or both.
-
Globus Pallidus: The “signal adjuster.” It fine-tunes the strength, like adjusting the volume on the radio.
-
Subthalamic Nucleus: The “emergency brake.” If something is too much, a sudden jerk, a repetitive motion, this slams on the brakes.
-
Thalamus: The “signal relay hub.” It’s the customer service desk, sending the final decision out to the body.
What “Movement Gating” Means for Everyday Actions
Now picture the walk sign at a busy corner. When everything’s working, the sign turns green or red on cue, no drama, no fuss. But if that light started blinking at random, you’d have a crowd of confused (and maybe cranky) pedestrians darting into traffic when they shouldn’t. With tics, the “movement gate” sometimes lets signals slip through out of turn. That’s why your kid might shout, blink, or twitch even when they’re trying not to.
The CSTC Loop Explained (Without Jargon)
The Loop in Simple Steps
Let’s break down this fancy phrase, cortico-striato-thalamo-cortical loop (CSTC pathway), without a headache. It’s a loop, like an amusement park monorail, shuttling signals in a circle:
-
Cortex (outer brain): Starts with an idea or urge (“pick up the pencil.”).
-
Striatum: Filters the idea, deciding if it should go further.
-
Thalamus: Passes the message along to the body’s movement teams.
-
Back to Cortex: Checks how things went, repeating or stopping as needed.
This loop is doing laps, constantly, fine-tuning everything from wiggling toes to facial expressions. In tic disorders, it’s like the circuit board picks up echoey feedback, signals get repeated even after they’re “done.”
Why “Feedback Loops” Can Repeat Movements
Ever heard that high-pitched whine when a microphone gets too close to a speaker? That’s feedback, a sound going in circles, louder and stronger, until someone turns down the dial. Your child’s brain can sometimes do the same. A movement urge gets let through the gate, but the signal bounces back, repeating itself until the circuit can finally quiet down. That’s why tics can happen over and over, even the same one, in a row.
How Misfiring in the Loop Becomes a Tic
Excitation vs Inhibition, The Gas and Brakes Metaphor
Time for a road trip metaphor: the brain has a “gas pedal” (excitation) and a “brake pedal” (inhibition). When you press the gas, you get movement: tap the brakes, and things stop. In tic disorders, especially when the basal ganglia aren’t balancing well, the brakes are a little loose. The result? Movements can speed through when you wish they wouldn’t.
The main action is in the striatum and thalamus (remember those from earlier?). That’s where the “gating” really happens; if the brakes are soft, the gate opens without enough control.
The Role of Dopamine Inside the Circuit
Here comes the chemistry. Dopamine, the brain’s supercharged fuel, makes movement possible, but too much or uneven dopamine makes traffic go haywire. Kids with Tourette’s or other tic disorders often have brain circuits awash in dopamine. This makes the movement loops super-sensitive, so the tiniest signal gets through (and might repeat).
Studies using Tourette’s brain imaging have shown irregular dopamine transport. The balance between dopamine and GABA (which acts as a brake, calming excess activity) is off. That’s why meds, supplements, or even nutrition tweaks (think zinc, magnesium, Omega-3s) sometimes show up in parent groups; folks want to influence these signals, hopefully making the “brakes” work better.
What Brain Imaging Studies Suggest (Parent-Level)
Patterns Researchers Often Look For
If you’ve wandered onto medical sites or parent forums, someone’s always talking about “MRI differences” or “PET scan findings.” Here’s what the science really shows:
-
Slight differences in the basal ganglia’s volume, not dramatic but measurable in groups.
-
Overactivation in those movement loops (motor CSTC circuit) and the limbic loop (emotion center)
-
Disrupted thalamic inhibition, which matches what we see in kids who just can’t stop a movement urge
It isn’t as wild as it sounds. These are patterns, not catastrophic damage or missing pieces.
Why Brain Scans Aren’t Usually Needed for Kids with Simple Tics
Here’s a breath of relief: for children with mild tics, pediatric neurology teams rarely order scans. Why? These patterns confirm what’s happening, but they don’t change the best way to help. Tics often get better with time, especially if you remove unhelpful triggers and offer a supportive environment. Observation and understanding your child’s unique patterns matter more than high-tech tests (plus, no expensive headaches down the road).

What Parents Can Observe at Home
Triggers That “Open the Gate”
Think about what throws your family’s routines out of whack: late nights, missed meals, launch-day video games, marathon screen sessions, and significant events. These are classic triggers for tics: stress, fatigue, excitement, and especially screen overstimulation.
Anecdotally, parents in Facebook groups swap stories of tics spiking at birthday parties or after a surprise fire drill at school. Some kids are like barometers; they signal “pressure” with tics that tick up faster than the weather changes in Texas.
Signs the Loop Calms Down
Ever watched your child utterly lost in drawing, building LEGO masterpieces, or making music? That deep focus, as it turns out, actually helps. Rhythmic activities, such as walking, swinging at recess, or even riding a bike, bring regulatory brain circuits online.
The sleep connection is real, too: those calm mornings after a good rest often mean fewer tics. If your child tends to “reset” after a swim or a long snuggle, that’s their brain’s way of finding calm, reminding you that it’s not just about problems, but about what restores balance.
Practical Supports That Help the Circuit Calm
Routines That Steady Brain Signals
A predictable rhythm to the day makes a world of difference. It’s all about keeping brain stress at a simmer, not a rolling boil. Here’s what families in tic disorder support forums swear by:
-
Consistent, adequate sleep, even on weekends
-
Hydration and regular meals, hangry brains = twitchy brains.
-
Scheduled movement breaks, like a short walk or five minutes on the trampoline between assignment chunks
-
Screen time limits (especially before bed)
And ditch those “boom-bust” days where you pack way too much in. (Been there, regretted it instantly.)
Behavioral Tools That Retrain the Loop
You might hear about CBIT, Comprehensive Behavioral Intervention for Tics, on sites like the Tourette Association, or in private Facebook parenting circles. CBIT teaches kids to spot the “itch” before a tic, then swap it for a less intrusive action, sort of like redirecting a sneeze into your elbow. It takes some practice (and a dash of humor), but many families see progress.
Pro tip: Some pediatric neurology clinics or occupational therapists offer CBIT coaching. Don’t be shy about asking, it’s not just for “severe cases.”
When to Talk to Your Clinician
If tics cause pain, keep your child from focusing at school, or make them anxious or embarrassed, it’s time to get a professional involved. The same goes if new or dramatic tics pop up suddenly or after an illness, think PANS/PANDAS. Pediatric neurologists (not just general pediatricians) are the right call for anything that seems out of the ordinary.
And if you’re not sure? You’re absolutely not alone. Most parents (including this one) have made at least one “am I overreacting?” call to the doctor.
Conclusion & Next Steps
You made it through the brain science obstacle course, with your sanity (hopefully) a little more intact. Remember, tics aren’t proof of a “broken brain.” They’re just a clue that your child’s brain circuit is running a little hot, kind of like a friendly laptop that just needs a reset, not a repair shop.
The good news? As those movement circuits mature and as your family finds routines that bring calm, many tics fade, or at least become a lot less overwhelming. It’s okay to mix expert advice with the tried-and-true recommendations from other parents. Don’t rule out support groups (forums, Facebook groups, the Tourette Association) when the days get tough or a consult with a functional medicine expert on tic disorders, if you’re stuck. Keep exploring gentle strategies, sometimes mindful movement, solid sleep, or a change in routine makes all the difference.
Still curious? Take a look at Dopamine GABA and Tic Disorders, and Tic Disorders and Sleep. One step at a time, you’ve got this.
If you are ready to dig deeper into your child’s tic disorder, click here and start with the Tic Disorder Cheat Sheet.
Frequently Asked Questions
The basal ganglia is a group of deep brain structures that act as a movement “gatekeeper,” deciding which movements to start or stop. In tic disorders, this system sometimes lets movements slip through unintentionally, resulting in sudden, repeated actions or sounds called tics.
The CSTC pathway (cortico-striato-thalamo-cortical loop) is a brain circuit that helps regulate movements. In tic disorders, miscommunication or feedback in this pathway can cause the same movement signal to repeat, making tics difficult to control.
No, tics are not a sign of brain damage. They reflect an overactive brain feedback loop, not injury or permanent problems. Most cases don’t require brain scans and can be managed with lifestyle changes and, if needed, behavioral interventions.
Yes, many children outgrow tics related to basal ganglia pathways as their brain circuits mature, particularly during puberty. Most tics become less frequent or less noticeable with time and supportive routines.
High-stimulation activities like video games can temporarily increase tics in some kids by ramping up dopamine and excitement. Taking regular screen breaks and monitoring how your child responds can help manage tic frequency.
Not at all. For many, lifestyle tweaks, behavioral training (like CBIT), and environmental changes are enough. Medication is there if tics are painful or disruptive, but it’s not the first (or only) solution.
A balanced diet, including healthy fats, magnesium, zinc, and Omega-3s, supports neurotransmitter balance in brain circuits like the basal ganglia. While some parents notice positive changes, always consult with a healthcare provider before starting supplements for tics.
This comes up daily in online parent groups. A balanced diet (think whole foods, enough healthy fats, magnesium, zinc, and Omega-3s) supports good neurotransmitter balance. Some parents report a difference with these nutrients, but always check with your child’s clinician before diving into supplements for Tourette’s Syndrome or persistent tic disorders.
els are too high or receptors are overly sensitive, it can trigger repeated movement signals, leading to tics such as eye blinking or shoulder twitching.
References:
Felling, R. J., & Singer, H. S. (2019). Neurobiology of Tourette syndrome: Current status and need for improved understanding. Movement Disorders, 34(7), 922–937. https://movementdisorders.onlinelibrary.wiley.com/doi/10.1002/mds.27702
Rozenkrantz, L., & Neeman, N. (2023). Structural and functional changes in Tourette syndrome. Behavioral Sciences, 13(8), 668. https://doi.org/10.3390/bs13080668
Xu, Y., Li, Y., Zhang, Y., & Wang, J. (2025). Prolonged screen time is associated with increased severity of tic symptoms in children with Tourette syndrome: A cross-sectional study. Italian Journal of Pediatrics, 51(1), Article 19. https://ijponline.biomedcentral.com/articles/10.1186/s13052-025-01851-w
Worbe, Y., Savulich, G., Voon, V., Houeto, J. L., & Robbins, T. W. (2018). Dopaminergic disturbances in Tourette syndrome: An integrative account. Molecular Psychiatry, 23(5), 1109–1119. https://www.nature.com/articles/mp2017139
Plessen, K. J., Bansal, R., Peterson, B. S., & Hedges, L. V. (2009). Meta-analysis of structural brain imaging in Tourette syndrome. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 33(7), 1129–1135. https://www.sciencedirect.com/science/article/abs/pii/S0278584609002048
Peterson, B. S., Thomas, P., Kane, M. J., Scahill, L., Zhang, H., Bronen, R., … & Leckman, J. F. (2003). Basal ganglia volume and tic severity in Tourette’s syndrome. American Journal of Psychiatry, 160(1), 149–155. https://psychiatryonline.org/doi/10.1176/appi.ajp.160.1.149
Wilhelm, S., Peterson, A. L., Woods, D. W., Piacentini, J. C., Deckersbach, T., Mink, J. W., … & Chang, S. (2024). Description, implementation, and efficacy of the comprehensive behavioral intervention for tics (CBIT): A narrative review. Journal of Child and Adolescent Psychopharmacology, 34(8), 477–488. https://doi.org/10.1089/cap.2024.0023
Liu, R., Duan, Y., Li, Y., & Wang, Y. (2022). Effects of group comprehensive behavioral intervention for tics in children with Tourette syndrome: A randomized controlled trial. Frontiers in Pediatrics, 10, Article 951340. https://doi.org/10.3389/fped.2022.951340

