When Jamie’s tics calmed after cleaning up the diet, her mom was floored. This wasn’t some steady progress or a benefit supplement, just a whole lot of fresh food, yogurt mornings, and a slow goodbye to sugary snacks. If that sounds too simple, you’re not alone. Most parents, maybe you, too, feel like they’re chasing shadows: one doctor after another, meds that work for a while, only to find tics roaring back at the worst possible times.
Does it ever feel like you’re the only one digging through Google at midnight, asking, “Could my kid’s tummy be driving these tics?” Or wondering if anyone has actually cracked this code?
Here’s the truth: there IS a quiet, robust conversation happening between your child’s gut and brain, and it matters. This isn’t some internet fad; it’s real biology, with real hope. In this guide, you’ll get the lowdown on the brain–gut connection in tics, how microbiome quirks might fan the flames, and step-by-step ideas to help the chaos settle, without resorting to expensive, one-size-fits-all “benefits.”
By the end, you’ll know why gut health is more than a wellness buzzword for families facing tics. You’ll walk away with practical ideas for meals, habits, and how to use probiotics for tics (without falling for hype). Let’s get started. You’re not alone in this; there’s hope, and it begins here.
Key Takeaways
-
The brain–gut axis plays a crucial role in the development and management of tics by connecting gut health and brain function.
-
Improving kids’ diets with fiber-rich vegetables, fermented foods, and less processed sugar can help reduce tic severity.
-
Gut bacteria influence brain chemicals like GABA and dopamine that are directly linked to motor tics and emotional balance.
-
Signs of gut imbalance, such as bloating, irregular stools, and skin issues, often occur in children with tics, highlighting the importance of microbiome health.
-
Introducing probiotics and prebiotics should be done gradually, with professional guidance and careful symptom tracking.
-
Everyday habits like better sleep, outdoor play, and family stress relief support a healthy gut–brain axis and can make a meaningful difference for children with tics.
Table of Contents
Getting Started: a Parent’s Story of Hope
Let’s rewind to the night Jamie’s mom sat in the dark, scrolling through stories of kids like hers. The usual advice, more meds, more waiting, just wasn’t cutting it. After yet another tough week at school, they’d both had it. “One more try,” she decided. So she swapped the toaster pastries for homemade yogurt parfaits, loaded the grocery cart with rainbow veggies, and added a splash of sauerkraut on the side (yes, she bribed her daughter with silly faces to try it).
A few weeks passed. Not every day was smooth. But the wild, up-and-down tics started to settle, a little calmer, fewer school calls, a whole lot less anxiety. It wasn’t magic. It was a gut-first plan. And it opened the door to a whole different way of tackling tics, one that doesn’t ignore what’s happening between the brain and the belly.
If you’ve dealt with frustrating doctor appointments, skeptical relatives, and confusing social media “benefit supports,” this story is yours. There is hope, and it’s more real (and more practical) than most people think.
Meet the Gut–Brain Axis
Ever heard your child say, “My tummy feels weird,” right before tics ramp up? Turns out, the gut and brain are chatty neighbors, practically sharing a secret hotline.
Vagus nerve, hormones, and immune messengers
Picture the vagus nerve as a superhighway. Most folks think the brain drives the show, but the truth is, for every message your brain sends to your gut, your gut sends back ten more. Wild, right?
But it’s not just nerves: there’s a hormone relay where gut cells pump out stuff like GLP-1 (helps with fullness), ghrelin (hunger), and immune messengers. These shape how the gut and brain “talk”: stress turns up, gut gets leaky, and suddenly tics can flare. And when we talk about inflammation, it isn’t just a fuzzy feeling; it’s mini-fireworks that wake up the movement part of the brain, making tics more likely.
This is real, not some “gut feeling.” Functional medicine leans into these two-way highways so we can help manage motor outbursts where they start.
Microbes that make brain-active compounds (GABA, serotonin precursors)
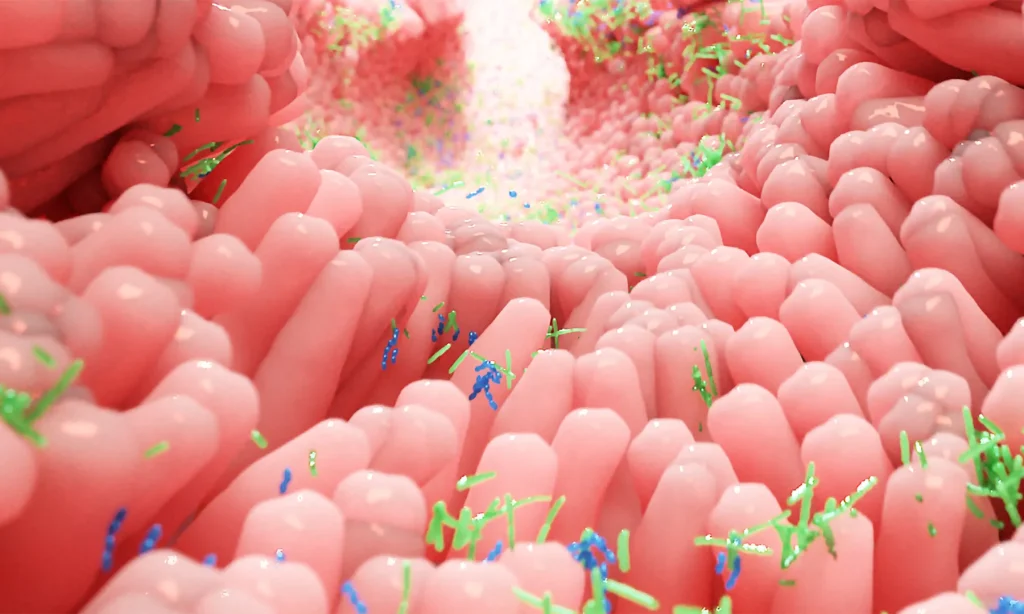
Let’s shrink down, microscope style: your kid’s gut is packed with trillions of bugs, bacteria, yeast, and even some friendly viruses. These tiny neighbors don’t just digest food. They help make brainy chemicals like serotonin (almost all of it), GABA (“brakes” for the nervous system), and the building blocks for dopamine.
If those bugs get out of whack (what the science folks call dysbiosis), the whole chemical conversation changes. More anxious days, more tics, and sometimes meltdowns that come out of nowhere. That’s the nutshell: the gut-brain connection, tics, your microbiome influencing mood, movements, and how your whole family feels day by day.
Dysbiosis: When the Microbiome Loses Balance
Common causes (antibiotics, ultra-processed foods, stress)
Here’s the secret of how food may be affecting tics: it’s not just about “bad bugs.” Dysbiosis happens when the good ones lose their edge. It’s shockingly common in kids with tics, way more than parents (and sometimes doctors) realize.
What throws things off? Repeat rounds of antibiotics (especially when little), a diet heavy in packaged snacks and colored cereal, and even good old-fashioned stress (school, family, the chaos of growing up). Add poor sleep or a stint with environmental toxins (hello, new carpets) and the scales really tip.
In functional medicine, we don’t just throw probiotics at the problem; we look at the whole system: food, sleep, life, and past medical history. Getting the entire picture is the only way to make a difference.
Signs in kids (bloating, irregular stools, skin issues)
Does your child get “bubble belly” after meals or skip the bathroom for days? Other gut red flags: bumpy rashes that come and go, wild mood swings, sudden sugar cravings, and more tics after eating. Sensory issues (hating tags, picky eating) sometimes tag along. And if your child has had lots of antibiotics, surprise infections, was born by C-section, or deals with ADHD or PANS/PANDAS, circle this section. They’re at higher risk for microbiome imbalances.
If you’re nodding along, it’s not all in your head. Dysbiosis can show up anywhere, from the toilet bowl to the classroom to the skin. Gut health is way more visible than we give it credit for.
How the Gut Influences Tics
SCFAs and inflammation: permeability (“leaky gut” idea explained carefully)
What happens when gut bugs go rogue? For starters, they stop making enough short-chain fatty acids (SCFAs), special compounds like butyrate and propionate. These molecules feed the cells lining your child’s gut, patch up leaks, cool off inflammation, and even send chills to overexcited brain circuits.
If diets are low in fiber (think: white bread, goldfish crackers, juice boxes instead of water), those SCFA levels nosedive. The gut lining gets patchy (some call this “leaky gut”), letting in things that kick off more inflammation. And guess what, brain cells tied to movement get crabby, and tics ramp up. The gut–brain axis hums on immune signals, not just happy hormones.
It’s a domino chain: more fiber and good bugs = more SCFAs = less inflammation = smoother days for your kid and your sanity.
Cross-talk with dopamine/GABA pathways (link to section above)
All these gut signals tap directly into the brain’s motor wiring, especially the dopamine and GABA channels. Kids with tic disorders (especially Tourette syndrome) have movement circuits that are a little jumpy.
Gut issues? They can seriously tip the scales by shifting dopamine sensitivity or lowering GABA (think: less brake, more gas). That quirky kiddo with a sensitive gut and wild tics? The microbiome might be a missing piece, not a random coincidence.
So, “managing gut health” isn’t some extra-credit project. It’s a main act for calming the movement music up top.
Parent-Friendly Food Patterns
Crowd-in fiber, colorful plants, fermented foods
Step one: don’t panic. Nobody’s asking you to bake sourdough from scratch or make every meal Pinterest-worthy. The trick is to “crowd in” the good stuff. Fiber-rich veggies (broccoli, red peppers, spinach), legumes, and whole grains feed those hungry gut bugs, kind of like compost for a thriving garden.
Fermented foods are the secret sauce. (Kids and fermented food? It’s possible, kefir smoothies with berries and spinach, carrot sticks dipped in hummus, or even pickles on the side.) Yogurt, kimchi, sauerkraut, and even kombucha can deliver beneficial microbes.
Fat and protein matter too: fatty fish (wild salmon), walnuts, pumpkin seeds, they all help both the brain and the bugs. Here’s a quick look at choices:
|
Include |
Avoid |
|---|---|
|
Leafy greens, veggies |
Sugary cereals, candies |
|
Fermented yogurt/kefir |
Soda, colored sodas |
|
Legumes, whole grains |
White flour snacks |
|
Salmon, walnuts, pumpkin seeds |
Fast food, cold cuts |
Pro tip: turning lunch into snack platters with something fermented and some crunch beats a brown bag any day.
Sample 3-day “calm-the-gut” menu framework (not medical advice)
If you’re feeling stuck about where to start, here’s a simple three-day framework (not a rigid plan, kiddo food drama is real):
Day 1
-
Breakfast: Plain kefir + berries + chia seeds
-
Lunch: Grilled salmon, quinoa, roasted broccoli, red bell pepper
-
Snack: Carrot sticks + hummus
-
Dinner: Lentil-veggie soup + salad with pickles
Day 2
-
Breakfast: Oatmeal with bananas, walnuts, and a hint of honey
-
Lunch: Turkey and avocado wrap (whole grain), cabbage slaw (fermented)
-
Snack: Apple + almond butter
-
Dinner: Stir-fry tofu + colorful veggies + brown rice, miso soup
Day 3
-
Breakfast: Scrambled eggs, spinach, toast, and kimchi on the side
-
Lunch: Chickpea salad (cucumber, tomato, olive oil)
-
Snack: Yogurt + pumpkin seeds
-
Dinner: Baked cod, sweet potato, asparagus, sauerkraut
Remember: This is about building habits, not grading yourself. Consult your doctor or a dietitian before making significant changes, especially if your child has food sensitivities or immune issues.

Probiotics & Prebiotics: What Families Ask
Food first vs supplements
Let’s get something straight: prebiotics are the plant fibers and veggie bits that feed “good” bugs. Probiotics are the actual microbes, which you can get from food or supplements. Fermented foods like yogurt and kefir offer a gentle start, since they’re familiar to most families and lower risk.
Are probiotic supplements the holy grail? Not exactly. Research on probiotics for tics is intriguing, but nobody’s found a benefit formula. Watch out for aggressive marketing, even in tic disorder forums; everyone swears by a different brand. Choose child-safe, third-party-tested, allergen-free blends. Start slow: half the recommended dose for a week, and always keep your clinician in the loop, especially if your kiddo has immune quirks or complex health needs.
How to introduce slowly and track changes
This isn’t a “splash and dash” fix. Here’s a sample tracking grid: Start date, brand/strain, dose, time (AM/PM)
-
Track each week: Tic frequency/severity, bowel changes, mood/energy, side effects.
-
Give each change at least 3–4 weeks for honest results.
-
If things go sideways, worse tics or bathroom drama, pause and ask for help.
Keep a family journal. It’s not about perfection, it’s about patterns. Pair this with tweaks to diet and routines for the best shot at calm.
For a deeper dive, you can check resources like Regenerating Health or trusted practitioners specializing in functional medicine for tic disorders.
Conclusion & Toolkit
Let’s tie all these ideas together into a “gut–brain routine” that takes the guesswork out of tic-friendly living. Here’s a handy checklist. Print it, post it on the fridge, share it in your parent group:
-
Eat fibre-rich veggies at every meal.
-
Include one fermented food daily (yogurt, kefir, pickled veggies)
-
Skip ultra-processed snacks, try real food for at least 3 weeks.
-
Introduce a probiotic (with your clinician’s blessing), track results
-
Make sleep and outdoor time non-negotiable.
-
Breathe/stretch/play when stress builds
Want to dive deeper into the brain-gut connection? Check out:
Remember, a healthy gut can change the game for tic disorders. This isn’t a replacement for your doctor, but it is a root-cause tool that makes your family’s journey smoother. There’s real hope in the gut–brain axis, and you’re right at the starting line.
Got more questions? Jump into a support group, such as Facebook groups, and find a specialist, or connect with Dr. Piper Gibson at Regenerating Health. Your family’s story can be one of hope, too.
If you are ready to dig deeper into your child’s tic disorder, click here and start with the Tic Disorder Cheat Sheet.
Frequently Asked Questions
The brain–gut axis is the communication network between the digestive system and the brain. In children with tics, this relationship matters because gut imbalances can influence brain chemistry and inflammation, potentially triggering or worsening tic symptoms.
Yes. Digestive issues like dysbiosis (microbial imbalance), leaky gut, or chronic inflammation can send stress signals to the brain. This may heighten sensitivity in areas that control motor tics. Addressing gut health through diet, probiotics, and lifestyle habits can help calm these responses.
Yes, research and parent experiences suggest that improving gut health through a diet rich in fiber, colorful vegetables, and fermented foods may help calm tics. Reducing processed foods and introducing gut-friendly habits often leads to noticeable improvements for many families.
Gut bacteria produce compounds that affect the brain’s mood and movement circuits. When there’s an imbalance (dysbiosis), it can disrupt these chemicals and lead to increased tics, anxiety, or mood swings. Supporting a balanced microbiome can make a difference in symptoms.
Gut microbes help produce neurotransmitters such as serotonin and GABA. When the microbiome loses balance, these chemical messengers can become dysregulated, potentially influencing tic frequency or severity. Restoring microbial diversity supports more stable brain–gut communication.
Fiber-rich vegetables, whole grains, legumes, fermented foods like yogurt and sauerkraut, and healthy fats from fish or seeds can nourish the gut microbiome. Avoiding processed snacks and sugary foods is also key to supporting a healthier brain–gut axis.
Probiotics from foods like yogurt and kefir are considered safe for most children and may support gut health, which links to tic management. Supplements should be introduced cautiously and under a doctor’s guidance, as individual results and needs vary.
Yes, both stress and poor sleep can disrupt gut health, leading to more tic flare-ups. Establishing calming routines, prioritizing sleep, outdoor play, and stress-reducing habits all help maintain a healthy brain–gut connection for children with tics.
Short-chain fatty acids (SCFAs) like butyrate are produced when beneficial bacteria digest dietary fiber. They reduce gut inflammation and strengthen the intestinal barrier, which protects the brain from inflammatory signals. Low SCFA levels have been linked to increased neurological sensitivity, including tics.
The vagus nerve acts as the main “information highway” between the gut and brain. It transmits signals that influence mood, digestion, and motor control. Strengthening vagal tone through relaxation, deep breathing, or outdoor activity can support calmer nervous-system responses and fewer tic flares.
Seek guidance from a clinician experienced in both neurology and functional medicine if tics worsen alongside digestive issues, skin problems, or mood changes. Comprehensive evaluation of diet, microbiome health, and inflammation can guide a safer, personalized plan.
References:
Hamamah, S., Aghazarian, A., Nazaryan, A., Hajnal, A., & Covasa, M. (2022). Role of microbiota-gut-brain axis in regulating dopaminergic signaling. Biomedicines, 10(2), Article 436. https://www.mdpi.com/2227-9059/10/2/436
Wang, Y., Xu, H., Jing, M., Hu, X., Wang, J., & Hua, Y. (2022). Gut microbiome composition abnormalities determined using high-throughput sequencing in children with tic disorder. Frontiers in Pediatrics, 10, Article 831944. https://doi.org/10.3389/fped.2022.831944
Vangay, P., Ward, T., Gerber, J. S., & Knights, D. (2015). Antibiotics, pediatric dysbiosis, and disease. Cell Host & Microbe, 17(5), 553–564. https://doi.org/10.1016/j.chom.2015.04.006
National Institute of Mental Health. (2025). PANS and PANDAS: Questions and answers. U.S. Department of Health and Human Services, National Institutes of Health. https://www.nimh.nih.gov/health/publications/pandas
Hamamah, S., Aghazarian, A., Nazaryan, A., Hajnal, A., & Covasa, M. (2022). Role of microbiota-gut-brain axis in regulating dopaminergic signaling. Biomedicines, 10(2), Article 436. https://www.mdpi.com/2227-9059/10/2/436
Wu, C.-C., Wong, L.-C., Hsu, C.-J., Yang, C.-W., Tsai, Y.-C., Cheng, F.-S., Hu, H.-Y., & Lee, W.-T. (2021). Randomized controlled trial of probiotic PS128 in children with Tourette syndrome. Nutrients, 13(11), Article 3698. https://doi.org/10.3390/nu13113698

