A twitch of the eye, an odd noise from the back seat, a shoulder shrug that just won’t quit, a parent knows when something’s off. But here’s a wild truth: underneath your child’s tics, there’s a tiny spark storming through their brain’s wiring, like an orchestra where the drums have lost the beat. And you’re not alone, so many parents watch, worry, and wonder if there’s something they missed.
What if, instead of a discipline issue or a mysterious habit, tics are your child’s brain having a communication glitch? It’s all about neurotransmitters, those microscopic messengers called dopamine and GABA. Forget the old myth that tics mean behavioral problems or “nerves.”
Ready for a fresh perspective, bust some myths, and get real, practical ways to help your child at home? Let’s unravel the rhythm of the brain, peek behind the curtain of movement, and figure out how small shifts can make a surprisingly big difference.
Key Takeaways
-
Dopamine and GABA imbalances are central to tic disorders, with dopamine increasing movement signals and GABA working as the brain’s calming brake.
-
Excess dopamine or reduced GABA can lead to more frequent or intense tics in children, highlighting the need for neurochemical balance.
-
Lifestyle changes, such as improving sleep, nutrition, and stress management, can naturally support healthy dopamine and GABA levels.
-
External factors like stress, poor sleep, certain foods, and some medications may trigger or worsen tic disorders.
-
Tracking daily patterns and seeking professional help when tics disrupt daily life can provide valuable insights and tailored support for managing tic disorders.
Table of Contents
Your Child’s Brain Has a Rhythm
Ever watched a jazz band where one musician suddenly goes offbeat? That’s a glimpse into what’s happening in your child’s brain during tics. Inside every brain, signals pulse, go, stop, repeat, rest, balancing movement, thought, and focus.
Here’s the secret: neurotransmitters like dopamine (the go-getter) and GABA (the master of chill) keep this rhythm steady. But when they’re out of sync, either too much gas, not enough brakes, those signals get scrambled.
Tics aren’t your child being willful. They’re just a result of these brain signals slipping off rhythm and understanding that? It’s the first step to genuine compassion, for you and your child alike. Learn more about the dopamine-GABA connection on our guide Neuroinflammation and Tics.
What Dopamine Does in a Healthy Brain
Dopamine’s Role: Motivation and Motion
Think of dopamine as your child’s brain fuel, like stepping on the gas pedal. It sends the “let’s go” signal, not just for movement, but also motivation and focus. In a brain running smoothly, dopamine tells the basal ganglia (this cool little hub that filters signals), the prefrontal cortex (the control center for focus and choices), and the motor pathways (responsible for moving muscles) to synchronize.
So, when dopamine is balanced, things… flow. Your child can focus on assignments, play tag, or pick up a toy without a second thought. Dopamine is the magic behind those moments when everything clicks.
In Balance
But what happens when that gas pedal goes from gentle cruise to lead foot? When dopamine is perfectly dialed in, your child’s movement, motivation, and attention don’t just work; they glide. It’s like a smooth ride on an open highway.
Most of the time, this natural dopamine balance is invisible. But when it tips too far, you start to see the engine revving out of control, and that’s when tics show up.
When Dopamine Levels Rise Too High
Overstimulation and Tics
Imagine pumping up the volume on your child’s brain radio until it’s blasting static; too much dopamine does just that. Those basal ganglia circuits go haywire, firing repeated “move” signals. Suddenly, your kid’s eyes are blinking on repeat, or their shoulders twitch without warning.
Can Too Much Dopamine Cause Tics?
Short answer: absolutely. Research shows that when dopamine is dialed up too high (or its receptors are way too sensitive), it floods the circuits with excess movement signals. It’s like your car’s accelerator getting stuck.
Clinical Insight
Here’s something most neurologists might not tell you: some meds for extreme tics (especially the old-school ones) aim to block or dampen dopamine to calm down all this overactivity. But that’s rarely the first path for natural-minded families, and it opens the door to exploring gentle rebalancing approaches instead.

Meet GABA: The Brain’s Calming Chemical
What Is GABA?
If dopamine’s the gas, GABA (gamma-aminobutyric acid) is your child’s brain’s brake pedal. It slows signals down, helps focus the mind, and reins in runaway thoughts and muscles. GABA and tics have an oddly tight bond. For some kids, low GABA activity means the brakes aren’t working so well, letting those involuntary movements sneak through.
GABA in Childhood Brain Development
During early years, when brain connections are forming lightning-fast, GABA steps in to help build circuits for movement, emotional control, and attention. Without enough GABA support, things get jumpy or scattered. Some of the calm, focused kids, you know? Thank their healthy GABA levels.
Deficiency Connection
It only takes a tiny dip in GABA to see the ripples. Studies show many kids with chronic tics have less GABA in the brain areas that control movement. It’s as if their brakes are just a little too soft, and the signals sneak through when they should stop.
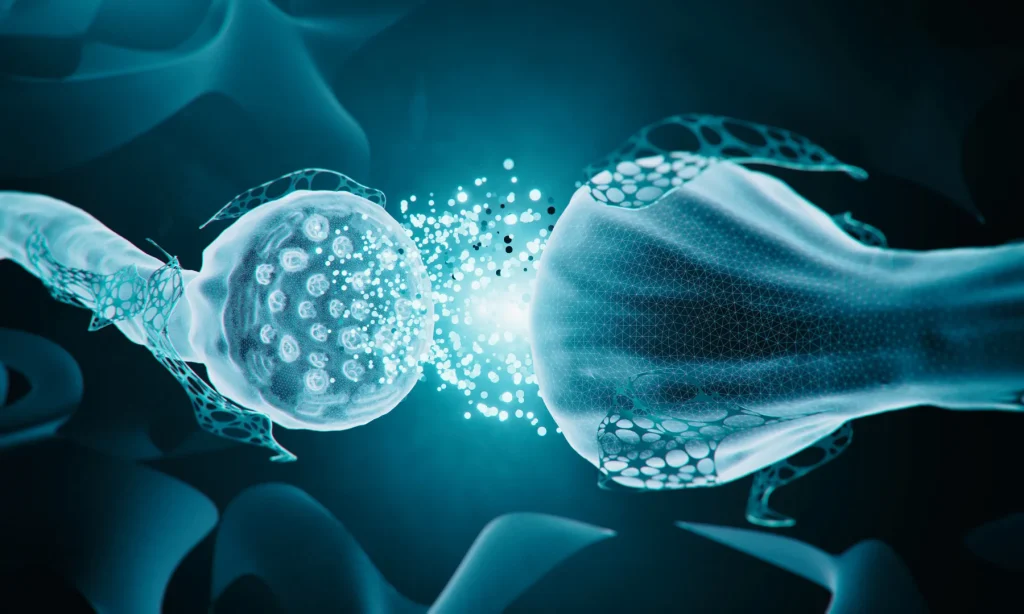
How GABA and Dopamine Work Together
Here’s where it gets wild: dopamine and GABA are like partners in a dance; when one dips, the other needs to adjust. If dopamine surges and GABA doesn’t, you get misfires. Picture it as a merry-go-round with one side spinning too fast while the other can’t keep up. That’s often what’s happening during a tic episode.
When these two are balanced, movement is smooth and intentional. But if the ‘go’ signal (dopamine) overwhelms the ‘brake’ (GABA), tics become the body’s way of handling that mixed-up rhythm, a sort of accidental engine backfire.
Parents chasing the perfect natural dopamine balance or looking for GABA support are really looking to smooth out this beautiful (if sometimes bumpy) dance.
What Research Shows About Tic Disorders and Neurotransmitters
Good news, science lovers: advanced brain scans (like MRS, the same tech in high-powered research labs) reveal fundamental differences in how brains with tics work. Kids and adults with Tourette’s and other tic disorders show higher dopamine receptor activity in the basal ganglia, the brain’s “traffic cop” for movement. That means they’re more sensitive to the very signal that can spark tics.
And it’s not just dopamine. Studies also find reduced GABA concentrations where movement control lives in the brain. Animal studies even show that ramping up dopamine triggers tic-like behaviors, but boosting GABA can slow them down.
Bottom line: the research backs up what parents see, when dopamine and GABA get out of sync, tics can appear. This isn’t theory; it’s the microbial effects on brain chemicals.
Factors That Influence Brain Chemistry in Kids
Stress
Ever notice tics get worse right before that big test, or after a rough day at school? Stress bumps up cortisol, which flips the switch on dopamine. For some sensitive brains, it’s like adding gasoline to a fire; tics pop up or get worse.
Sleep
Sleep isn’t just beauty rest for kids; it’s when the brain recycles neurotransmitters after a day of traffic. Cut sleep short, and you’re asking for more tic trouble.
Nutrition
Food fuels the neurotransmitters behind your child’s every thought and twitch. Protein-rich meals provide the building blocks for dopamine, while B-vitamins and magnesium keep GABA humming. Skimp here, and the brain’s rhythm gets wobbly.
Inflammation
Chronic inflammation (from illness, allergies, or even gut glitches) plays tug-of-war with dopamine pathways and can light up tic activity. If your child has a sensitive tummy or frequent colds, it’s worth looking into.
Medications
Some meds, especially stimulants for ADHD, can tip the natural balance, making tics more frequent. Always chat with a pediatrician or functional medicine doc if you’re seeing new tics after starting a med.

Supporting a Healthy Neurochemical Balance at Home
Let’s be real: if telling a child to “stop” a tic worked, none of us would be here. But there are ways to gently nudge the brain’s rhythm back on track, right in your own home.
Prioritize Restorative Sleep
-
Set a soothing bedtime routine (snuggly PJs, soft lights, a calming story).
-
Say no to screens 60 minutes before bed. (The blue light tricks the brain’s sleep clock.)
-
Give your child time to wind down, even if it means an extra hug.
Focus on Nutrition
-
Offer meals rich in protein, leafy greens, and nuts. They feed the neurotransmitters.
-
B-vitamins and magnesium are GABA’s best cheerleaders, think eggs, beans, sunflower seeds.
-
Omega-3s (from salmon, walnuts, or a quality supplement) fight inflammation and help keep those brain signals smooth.
Encourage Physical Movement
-
Movement is medicine. Swimming, biking, or yoga can naturally boost both dopamine and GABA; keep it fun.
-
If your child hates sports, try daily nature walks. Even five minutes helps.
Manage Emotional Stress
-
Try the “Hot Cocoa Breathing” trick: in through the nose, out slow like cooling cocoa. It calms the whole nervous system.
-
Practice gratitude or calming affirmations at bedtime.
Avoid Overstimulation
-
Limit high-sugar snacks, sodas, and marathon video game sessions; these can spike dopamine and make tics worse.
Pro Tip: Keep a tic diary. Jot down what they ate, slept, did, and how the tics changed. Patterns often hide in the details.
When to Seek Professional Guidance
Sometimes, tics go from quirky to concerning. If they’re making school hard, stealing sleep, or if they show up with big mood swings, anxiety, or OCD, it’s time to bring in the experts.
Partner with clinicians, like those at Regenerating Health, who see the whole child, not just the indicator. Ask about brain-training therapies, dietary changes, or options besides traditional tic – if that’s your family’s vibe. (There are amazing communities and Facebook groups where parents share their own journeys; don’t be shy to connect.)
You know your child better than anyone. Trust that gut if you feel something’s just not right.
Tic disorders aren’t a sign of broken brains; they’re a sign that your child’s internal orchestra needs a little extra help tuning its instruments. The dopamine-GABA balance isn’t set in stone: it shifts as your child grows, learns, and heals.
Supporting your child isn’t about magic pills or quick fixes. It’s about small, meaningful changes, restful sleep, nurturing meals, joyful movement, a calm space, and finding supportive professionals who really listen
If you are ready to dig deeper into your child’s tic disorder, click here and start with the Tic Disorder Cheat Sheet.
Frequently Asked Questions
Yes, and it can do a number on tics. Sugar surges temporarily spike dopamine, so for sensitive kids, that means more risk of brain static and tic flare-ups. You might spot a pattern of tics shortly after birthday cake or soda.
GABA supplements may not always cross into the brain as needed. Some families use alternatives like magnesium glycinate or L-theanine for natural support, but it’s best to consult a healthcare professional before starting any supplement.
Many children outgrow dopamine-related tics as their brains mature and better regulate neurotransmitters. A supportive environment with healthy routines can help smooth this process, although some may need professional guidance.
Dopamine and GABA are neurotransmitters that influence movement and brain rhythm. High dopamine can overstimulate movement signals, while low GABA means less ability to slow those signals. An imbalance between them often leads to the appearance of tics in children.
Dopamine acts as the brain’s ‘go’ signal. When dopamine levels are too high or receptors are overly sensitive, it can trigger repeated movement signals, leading to tics such as eye blinking or shoulder twitching.
Yes, research shows that children with chronic tics often have lower GABA concentrations in brain areas controlling movement. Low GABA means the brain’s ‘brakes’ are weaker, letting involuntary movements or tics occur more easily.
Supporting a healthy neurotransmitter balance includes prioritizing sleep, providing protein-rich meals with leafy greens and nuts, supplementing with B-vitamins and magnesium, encouraging physical activity, reducing stress, and avoiding overstimulation from sugar and excessive screen time.
References:
Maia, T. V., & Konkoly, C. (2018). Dopaminergic disturbances in Tourette syndrome: An integrative account. Biological Psychiatry, 84(5), 332–344. https://www.biologicalpsychiatryjournal.com/article/S0006-3223(18)31300-3/abstract
Wong, D. F. (2002). Elevated intrasynaptic dopamine release in Tourette’s syndrome measured by PET. American Journal of Psychiatry, 159(8), 1329–1336. https://psychiatryonline.org/doi/10.1176/appi.ajp.159.8.1329
Puts, N. A. J., Harris, A. D., Crocetti, D., Nettles, C., Singer, H. S., Tommerdahl, M., Edden, R. A. E., & Mostofsky, S. H. (2015). Reduced GABAergic inhibition and abnormal sensory symptoms in children with Tourette syndrome. Journal of Neurophysiology, 114(2), 951–963. https://doi.org/10.1152/jn.00060.2015
Adams, J., Trolese, M. C., Varrone, A., & Schwarzbold, M. L. (2018). Striatal dopaminergic alterations in Tourette’s syndrome: A meta-analysis based on 16 PET and SPECT neuroimaging studies. Translational Psychiatry, 8(1), Article 190. https://doi.org/10.1038/s41398-018-0202-y
Mogwitz, S., & Roessner, V. (2018). Update on the pharmacological treatment of tics with dopamine-modulating agents. ACS Chemical Neuroscience, 9(4), 651–672. https://doi.org/10.1021/acschemneuro.7b00460
Adam, R., Miall, R. C., Brown, M. W., & Vogt, B. A. (2003). Increased ventral striatal monoaminergic innervation in Tourette syndrome. Neurology, 61(4), 476–482. https://doi.org/10.1212/01.WNL.0000076181.39162.FC
Freed, R. D., Wu, M., McPhee, D. J., Eilbott, J. A., McGinnis, E., Ramamurthy, S., Yang, J., Shungu, D. C., & Gabbay, V. (2016). Decreased anterior cingulate cortex γ-aminobutyric acid in youth with Tourette’s disorder. Pediatric Neurology, 65, 64–70. https://doi.org/10.1016/j.pediatrneurol.2016.08.017
Cadeddu, R., Knutson, D. E., Mosher, L. J., Loizou, S., Odeh, K., Fisher, J. L., Cook, J. M., & Bortolato, M. (2021). The α6 GABAA receptor positive allosteric modulator DK-I-56-1 reduces tic-related behaviors in mouse models of Tourette syndrome. Biomolecules, 11(2), Article 175. https://doi.org/10.3390/biom11020175