Could mast cell activation be the hidden trigger behind tics?
When mast cells in your immune system go into overdrive, they release too many chemicals. Those chemicals can irritate your nervous system and worsen your tics. Understanding mast cells, their overdrive, and the connection to tic development might uncover some surprising truths about the nature of these neurological disruptions.
Key Takeaways
Mast Cell Activation Syndrome (MCAS) can trigger inflammation that impacts the nervous system, potentially worsening tics.
Overactive mast cells release chemicals that disrupt dopamine signaling and may contribute to neurological signs like motor and vocal tics.
Factors such as genetic predispositions, gut imbalance (dysbiosis), and environmental triggers can exacerbate mast cell dysfunction and tic symptoms.
Managing MCAS involves identifying triggers, adopting an anti-inflammatory diet, incorporating supplements like quercetin and vitamin C, and controlling environmental irritants.
Stress management, gut health improvement, and holistic approaches tailored to the child’s unique needs can support reduced tics and better overall well-being.
Seeking help from specialists, including pediatric neurologists, allergists, and therapists trained in behavioral therapy, provides crucial support for managing tics effectively.
Table of Contents
Understanding Mast Cell Activation Syndrome (MCAS)
When your child exhibits neurological tics, it’s natural to seek answers. One overlooked factor could be Mast Cell Activation Syndrome (MCAS), in which the immune system becomes overly reactive, creating far-reaching effects on the body and brain.
What Is MCAS?
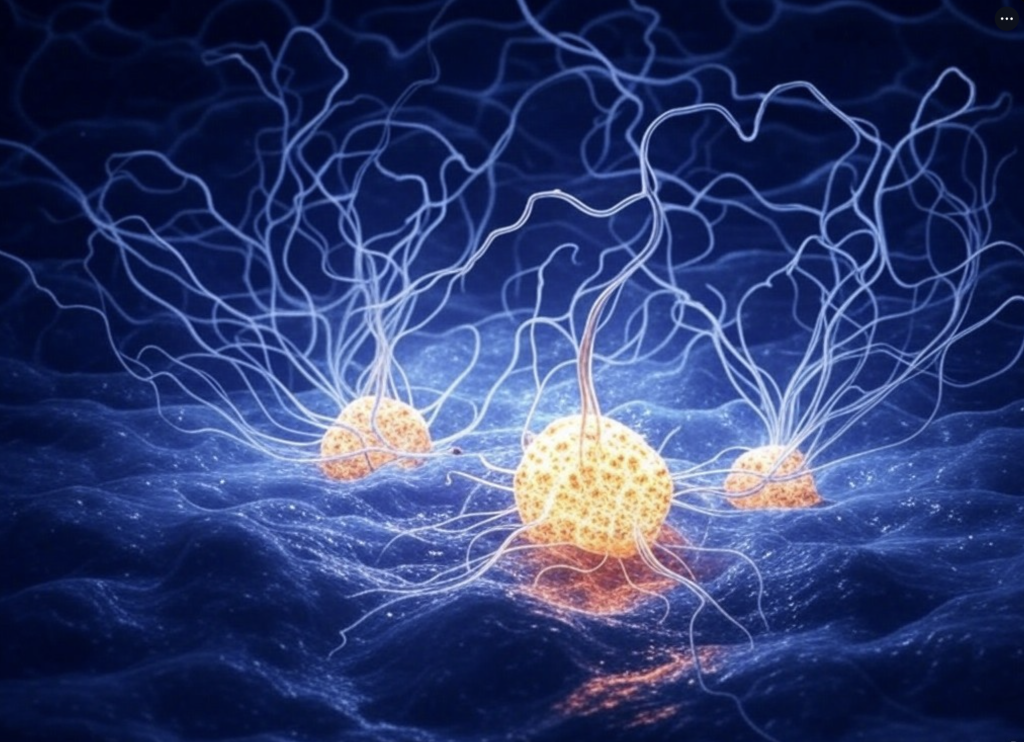
When mast cells—part of the immune system’s frontline defense—go into overdrive, mast cell activation syndrome occurs. Instead of releasing chemicals like histamines, prostaglandins, and cytokines in regulated amounts to combat infections or fine-tune healing, these cells dump out an uncontrollable amount of inflammatory materials. Hence, an MCAS person has a hypersensitive nervous system and body. Persistent inflammation is the MCAS and becomes the body’s “new normal”.
In MCAS, mast cells lose the usually well-tuned balance between protection and repair. They respond over actively to subtle triggers, and the immune system is constantly under attack—mounting an army—but there is no serious threat to mobilize against.
Signs of MCAS
Signs of MCAS often feel like an unsolvable puzzle, with pieces scattered across different systems in the body. Clues can include chronic inflammation, rashes, or digestive problems, but neurological signs like tics might also emerge. These subtle connections often escape notice because MCAS isn’t just about allergies.
The overactivation of mast cells can result in:
Sudden allergic-like reactions to foods, scents, or environmental changes.
Persistent itchiness, headaches, or muscle discomfort without a clear cause.
Neurological signs like increased vocal or motor tics seem to come and go unpredictably.
When inflammation caused by these chemicals affects the brain, it disrupts normal neurological functioning. This vital detail links MCAS to tic disorders and highlights the need for targeted management.
The Connection Between MCAS and Tics
Overactive mast cells release substances that create neural inflammation, subtly altering the delicate environment in your child’s brain. This inflammation can irritate pathways responsible for the smooth processing of motor and vocal functions, amplifying tics. While sneaking through these pathways, rogue mast cells may also open weak points in the blood-brain barrier, letting harmful agents slip into brain tissue.
Disrupted dopamine signals add another twist. Dopamine, often called the brain’s motivator, controls movement and focus. Mast cell chemicals can throw this system off balance, fueling movements like tics. Imagine watching a ripple move across still water; mast cell activity creates similar disruptions but over neural circuits.
These intricate connections might explain why confident kids with unexplained, worsening tics may find relief only after addressing immune system triggers. Managing MCAS involves identifying the culprits—foods, environmental toxins, or emotional stressors—and reducing their impact to restore calm inside this biochemical storm.
Why Do Mast Cells Become Overactive?
When mast cells misbehave, they release inflammatory chemicals that disrupt your child’s body and mind. Understanding why this happens is key to calming the chaos and finding relief. Overactivity doesn’t occur in isolation; it’s often a puzzle with multiple contributing pieces.
Comorbidities to Consider
Your child’s other health conditions might be fueling mast cell dysfunction. Chronic allergies, autoimmune disorders, and gut imbalances can overstimulate the immune system, pushing mast cells into overdrive. For example, if gut bacteria are out of balance, the immune system might see harmless substances as threats, forcing mast cells to step into action. Similarly, persistent allergies can create a cycle of inflammation, keeping mast cells on high alert. The connection between these conditions hints at how sensitive the immune system can become in children with tics or neurological signs.
Genetic Predispositions
Some children seem born with an unfair advantage—if that advantage were overactive mast cells. Genetics can play a significant role. If other family members deal with immune system irregularities, allergies, or even MCAS, your child might have inherited a predisposition for mast cell dysfunction. It’s not destiny but a vulnerability written in their DNA. Imagine a switch halfway turned on; environmental triggers, stress, or illness might be all it takes to push those mast cells into full activation.

The Gut-Brain Connection
Your gut and brain are in constant conversation, and this dialogue plays an important role when managing conditions like MCAS and tics. The gut isn’t just where food is digested; it’s home to trillions of bacteria that influence your entire body, including the nervous system. When this ecosystem becomes imbalanced, known as dysbiosis, it can spark a chain reaction—an overactivation of mast cells.
Mast cells, like vigilant guards, respond to threats. But when dysbiosis occurs, these cells may misinterpret signals, triggering unnecessary inflammation. This inflammation isn’t contained; it can travel, affecting other systems. Neuroinflammation—the brain’s immune response—can escalate, intensifying tics or other neurological signs.
Imagine a highway connecting your gut and brain. The vagus nerve carries messages both ways. If inflammation blocks the route, communication falters. Your child’s brain may interpret these faulty signals as stress or threat, provoking changes in behavior or worsening tics.
Improving gut health restores balance to this intricate system. Addressing dysbiosis and reducing gut inflammation may have a ripple effect: calmer mast cells, reduced neuroinflammation, and fewer neurological disruptions.
Strategies for Managing MCAS and Reducing Tics
Understanding the dynamic between mast cells and tics reveals actionable ways to manage signs. Small, consistent changes to your child’s lifestyle can ease the burden of MCAS and its neurological effects.
Identifying Triggers
Patterns hide in the chaos of signs. Keeping a food and indicator journal acts like a magnifying glass. By tracking what your child eats, you can uncover hidden triggers. Their favorite snacks might be aged cheeses, citrus fruits, or artificial dyes. This habit creates a roadmap to avoid inflammation-triggering culprits in their routine.
Dietary Changes
The foods on your child’s plate hold power. Reducing histamine-rich options, like processed meats and fermented favorites, lightens the load for overactive mast cells. Instead, lean into an anti-inflammatory diet. Brightly colored fruits, leafy greens, and omega-3-rich fish provide essential nutrients while calming internal fires. Imagine their plate as a canvas, each choice contributing to a more balanced system.
Supplements for Stabilizing Mast Cells
Certain compounds work behind the scenes to stabilize mast cells. Quercetin found naturally in apples and onions, and vitamin C, abundant in oranges and bell peppers, act like calming agents. With your healthcare provider’s guidance, adding these supplements supports less reactive mast cells. They’re like steady hands, easing unpredictable responses.
Environmental Control
The air around your child matters. Reducing exposure to synthetic fragrances, cleaning chemicals, and hidden molds removes daily irritants. Think of your home as an oasis where triggers don’t follow. Frequent dusting, using non-toxic cleaners, and maintaining good ventilation create a sanctuary for your child’s sensitive system.
Stress Reduction
Stress whispers loudly to mast cells. Practicing mindfulness activities, like deep breathing or yoga, interrupts the noise. Encourage regular playtime outside—running, jumping, and laughter work wonders for their immune balance. These moments, woven into their day, act not as quick fixes but as steady rhythms, helping the body manage its reactions.
Taking a Holistic Approach
Addressing conditions like tics and mast cell activation requires looking at the bigger picture. While medical treatments can help, adopting a holistic strategy can help manage symptoms and improve overall quality of life.
Personalized Solutions
Every child’s journey with tics or conditions like PANS/PANDAS is unique. Rather than relying on one-size-fits-all approaches, consider solutions tailored specifically to your child’s needs. Work with specialists to identify triggers that exacerbate signs. For example, eliminating food sensitivity, such as gluten intolerance, might reduce an overactive immune response. Similarly, environmental allergens, like dust mites or pet dander, can be minimized to create a more stable environment.
Some children respond positively to anti-inflammatory diets, while others may benefit from targeted supplements like omega-3 fatty acids or probiotics. Your child’s immune profile, gut health, and lifestyle should guide decisions. A combination of strategies often yields the best outcomes, but identifying the right mix requires patience and a detailed understanding of your child’s needs.
How to Get Help with Tics
Seeking support starts with the right team. If you’re a parent looking for guidance on managing your child’s tics, consider booking a free consultation with us. We can help identify potential triggers, recommend personalized strategies, and provide the support you need to navigate this journey. Don’t hesitate to take the first step toward understanding and addressing your child’s needs.
Conclusion
Understanding the link between mast cell activation and tics opens new possibilities for managing these challenges. You can take meaningful steps toward relief by exploring potential triggers, supporting gut health, and adopting calming lifestyle changes.
Every child is unique, so finding what works best requires patience and collaboration with specialists. Remember, you’re not alone in this journey. There’s a growing community of families exploring similar paths. Small changes can make a big difference.
References:
Afrin, L., Self, S., Menk, J., & Lazarchick, J. (2016). Characterization of Mast Cell Activation Syndrome. The American Journal of the Medical Sciences, 353, 207–215. https://doi.org/10.1016/j.amjms.2016.12.013.
Brock, I., Prendergast, W., & Maitland, A. (2021). Mast cell activation disease and immunoglobulin deficiency in patients with hypermobile Ehlers‐Danlos syndrome/hypermobility spectrum disorder. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 187, 473 – 481. https://doi.org/10.1002/ajmg.c.31940.