Imagine noticing your child blink, twitch, or make sounds they can’t control. At first, you might brush it off as a phase, but over time, those little patterns grow harder to ignore. These are more than random habits; they’re signs of tic disorders, and understanding them can be the first step toward real answers.
The challenge isn’t just the tics themselves; it’s the uncertainty that comes with them. What are the triggers? Why do some children experience mild, passing tics while others face more severe, lasting conditions like Tourette’s? And most importantly, how do you move beyond labels to find what’s really driving the problem?
This guide will unpack tic disorders and the spectrum through a different lens: one that looks for root causes, not just surface symptoms. By the end, you’ll have a clearer picture of what’s happening beneath the surface and how a holistic approach can offer your family both clarity and hope.
Key Takeaways
-
Tic disorders exist on a spectrum, ranging from mild, temporary tics to complex conditions like Tourette’s Syndrome, and often overlap with other spectrum disorders such as ADHD and ASD.
-
Understanding root causes such as environmental toxins, gut health, and emotional stress can provide insight into managing and reducing tics effectively.
-
Functional medicine emphasizes testing for hidden triggers (e.g., mold, food sensitivities, heavy metals) to craft personalized solutions, rather than relying on guesswork.
-
Holistic approaches such as dietary changes, stress management, movement, and mindfulness techniques can significantly improve symptoms and overall well-being.
-
Labels like “Tourette’s” or “ADHD” should be seen as tools to guide care, not limit potential, as addressing the whole child often yields better outcomes.
-
Many myths about tics, such as being uncontrollable or untreatable, are false. Early intervention, tailored strategies, and patience can help children thrive.
Table of Contents
Breaking Down Tic Disorders and the Spectrum
Tic disorders can feel like a puzzle with too many pieces that just don’t fit. You might’ve noticed your child blinking excessively, making sudden noises, or doing repetitive movements—completely involuntary! These behaviors, called tics, can range from minor distractions to signs of conditions like Tourette’s syndrome. So, where do tic disorders sit on the “spectrum”? Let’s immerse.
What Does “Spectrum” Mean?
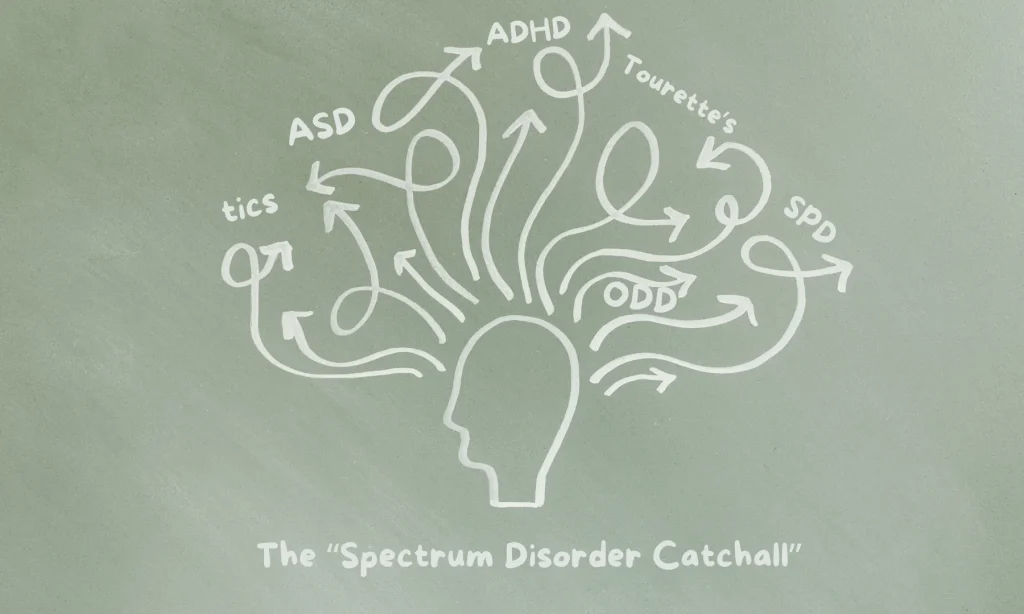
When experts talk about a spectrum, they’re describing a range of conditions that share overlapping traits. Tic disorders, including Tourette’s, often get mentioned alongside Autism Spectrum Disorder (ASD), Attention-Deficit Hyperactivity Disorder (ADHD), Sensory Processing Disorders (SPD), and even Oppositional Defiant Disorder (ODD). Why? Children with these conditions often face similar challenges, including repetitive behaviors, difficulty with focus, and social interactions.
But it’s not a one-size-fits-all label. Just because disorders have overlapping traits doesn’t mean they’re identical. Think of it like comparing siblings: they may share features, but they’re unique in how they “show up.”
Tic Disorders vs. Other Spectrum Disorders
Tic disorders stand out because the tics themselves are physical behaviors, such as head jerking or throat clearing, that your child can’t control. In contrast, other spectrum disorders like ASD often involve social and communication issues. The connection between them is more about shared struggles than shared causes. And honestly, that’s where some of the confusion (and frustration!) comes in for parents.
For instance, your child with Tourette’s might also have ADHD traits, like the inability to sit still. Or maybe sensory sensitivities (tags in clothes feeling unbearable) remind you of what you’ve heard about ASD. Dr. Piper Gibson, who specializes in natural approaches to tics at the Tic Disorder Institute, points out that many families see overlaps. These similarities can make exploring the diagnostic process tricky, but also help paint a fuller picture of what’s going on.
Why Does Labeling Matter for Parents?
The idea of the spectrum can be overwhelming. But understanding how tic disorders relate to this broader concept helps you advocate for your child. Whether it’s talking to schools, therapists, or other parents, you need clarity. Labels aren’t about boxing kids in; they’re about figuring out what support works best for them.
For kids with tics, mislabeling can cause unnecessary stress. If someone assumes repetitive behaviors are “just ADHD” or part of a “phase,” they might miss signs of something more complex, like Tourette’s. This is why you’re the expert on your child, you know what’s a quirk, what’s a tic, and when it’s time to dig deeper.
The Debate Over the Spectrum Approach
Not everyone agrees on grouping tic disorders onto a spectrum. Some argue it oversimplifies complex conditions. Others worry it makes disorders harder to understand, throwing parents into a whirlwind of guesswork. But it also makes sense: with so much overlap in signs, recognizing shared challenges can lead to tailored strategies that actually help.
When we talk about “tics and the spectrum,” it’s not about adding pressure to identify a million things at once. It’s about seeing the fuller picture, connecting dots, and supporting kids the way they deserve.
Beyond Labels: Why We Must Look Deeper
When your child’s life starts revolving around tics, the labels can feel overwhelming—Tourette’s, PANS, PANDAS, ADHD. What if, instead of getting caught in the thick forest of diagnoses, you took a step back to uncover the root causes? It’s about more than sticking a name on the signs; it’s understanding why those signs are there in the first place.
Ask “Why,“ Not Just “What”
It’s easy to accept a recognition at face value. Your child has tics? It must be Tourette’s, right? But up to 1 in 4 children in the U.S. struggle with a chronic condition, and many of these are interconnected. From the gut-brain connection to environmental toxins, there might be unexpected factors quietly driving those tics. Have you noticed patterns, like tics flaring after illness or stress? These clues can be as crucial as any label.
Focus on the Whole Picture
Sleep, diet, stress, even hidden infections (like strep with PANS/PANDAS), they all play their part. If you only look at one piece, you’ll miss the bigger picture. Sometimes, it’s the food they eat or those artificial colors in snacks. Other times, it’s about calming an overwhelmed nervous system. Moving beyond labels often means asking: “What’s throwing things off balance?”
Stop Defining by Recognition
Spectrum disorders like tics and ADHD come with heavy baggage—possibly even stigmas. But your child is more than their tics. Labels should guide care, not become a box that limits potential. When you dig deeper, you can help your child thrive in ways these words might’ve never suggested.
Think of Labels as Entry Points
Instead of end-all answers, think of diagnoses as starting points. They give you a direction to explore: it can be finding a specialist, like someone at the Tic Disorder Institute, or diving into natural remedies for relief. There’s no one-size-fits-all solution, but taking the longer road often means uncovering answers textbooks won’t have.
So, where should you start? Maybe by challenging the first label you’re given. The deeper you dig, the closer you’ll get to revealing solutions that actually make a difference.

The Perfect Storm Behind Tic Disorders
Tic disorders rarely have a single cause. More often, they appear when several factors overlap: environmental exposures, biological imbalances, physical habits, and emotional stressors. Understanding how these triggers interact is key to managing tics effectively.
Environmental Factors
Children are exposed daily to pesticides, household chemicals, food additives, and synthetic products. This “toxic load” can overwhelm developing systems. For example, glyphosate has been linked to gut disturbances that affect brain function, while artificial dyes and preservatives can worsen tics in sensitive children.
Practical step: Choose organic when possible, reduce processed foods, and check labels for unnecessary additives.
Biological Factors
The gut and brain constantly communicate: signals from the gut outnumber those from the brain ten to one. Conditions like leaky gut, food sensitivities (gluten, dairy), mold exposure, or hidden infections (such as strep in PANDAS) can trigger inflammation and worsen tics.
Practical step: Trial elimination of common irritants like sugar or artificial sweeteners, and consider professional testing for sensitivities or gut imbalances.
Physical Factors
Modern routines limit natural movement. Long periods of sitting, poor posture, and excessive screen time restrict circulation and reduce the body’s ability to regulate stress, both of which can influence tics.
Practical step: Encourage daily activity, such as walking, playing outdoors, or taking short movement breaks. Consistency matters more than intensity.
Mental & Emotional Factors
Stress, whether from school, social pressures, or disrupted routines, often amplifies tics. Even lack of sleep can worsen symptoms.
Practical step: Establish calming routines such as deep breathing, reading together before bed, or short mindfulness exercises. If stress feels unmanageable, seek support from a therapist experienced in tic disorders.
Functional Medicine’s Approach: Test, Don’t Guess
Sometimes it feels like you’re stumbling in the dark when trying to understand your child’s tics, right? That’s where functional medicine steps in. Instead of stopping at surface-level signs, it asks the deeper question: what’s causing them in the first place?
This approach shifts the focus from labels and quick fixes to uncovering triggers that might be hiding beneath the surface. Conventional visits often overlook things like mold exposure, heavy metals, or candida overgrowth, yet these can dramatically influence tic disorders and the spectrum of related conditions.
By choosing to test, not guess, you’re refusing to settle for band-aid solutions. Testing shines a light on underlying imbalances and connects them to real-world struggles, whether it’s vocal tics that flare unexpectedly or motor tics that worsen under stress. Instead of random trial and error, you get a clear map of what’s happening in your child’s body.
Functional medicine isn’t about a one-size-fits-all answer. It’s about solving a puzzle, piece by piece, until you see the bigger picture of what’s driving your child’s tics. That clarity is what empowers you to move forward with confidence.

Step-by-Step Healing Framework to Manage Tic Disorders Holistically
Once you understand the philosophy behind functional medicine, the next step is putting it into action. Dr Piper Gibson specializes in uncovering the root cause of tic disorder symptoms and creating a holistic plan for your child. Here’s a practical roadmap to guide you:
Step 1: Identifying Tic Disorder Triggers Through Testing
Think of your child’s tics like a flashing “check engine” light. Ignoring it won’t help, and running one quick test won’t tell you the whole story. That’s why comprehensive testing is the foundation. This might include evaluating for hidden triggers such as mold, heavy metal toxicity, gut imbalances, infections, or food sensitivities. A neuro-immune evaluation gives you that big-picture view.
Step 2: Linking Test Results to Tic Disorder Symptoms
Test results are only helpful if you understand their real-life implications. This stage is about translating data into insight. For example, if mold toxins show up on a lab report, it may explain sudden flare-ups of vocal tics. If food sensitivities appear, they may be tied to blinking or shoulder-jerking tics. Every clue builds a clearer link between biology and behavior.
Step 3: Creating Your Child’s Custom Tic Disorder Recovery Plan
Armed with the insights, it’s time to take action. A tailored plan could mean adjusting diet to repair gut health, creating a toxin-free home environment, supporting stress resilience, or using targeted supplements. Recovery isn’t instant—it takes patience. A helpful rule of thumb: expect one to two months of healing for every year your child has had symptoms.
Strategies That Work in Real Life
-
Reduce Exposure to Environmental Toxins – swap cleaners, go organic where possible, limit pesticides.
-
Support Gut Health – add probiotics, fermented foods, and fiber while cutting sugar and processed snacks.
-
Build Movement into Everyday Life – encourage play, exercise, and outdoor time to regulate stress and energy.
-
Address Emotional Stressors – create safe spaces, introduce mindfulness, and check for hidden school or social stress.
-
Test for Hidden Triggers – revisit testing if progress stalls; don’t assume the first round caught everything.
-
Holistic Remedies – calming baths, essential oils, or relaxation techniques can provide extra support.
-
Join Supportive Communities – connect with other parents walking the same path for encouragement and tips.
-
Take an Incremental Approach – implement changes step by step to avoid overwhelm and ensure consistency.
Managing the Perfect Storm with Holistic Solutions
Tic disorders can feel overwhelming, but they don’t define your child or their future. By focusing on the bigger picture and digging into root causes, you can uncover meaningful ways to support their well-being. Small, intentional changes in areas like diet, environment, and stress management can make a real difference over time.
You don’t have to navigate this journey alone; working with a functional medicine expert on tic disorders will help your child manage tics and thrive. Trust the process, celebrate progress, and remember hope is always part of the equation.
If you are ready to dig deeper into your child’s tic disorder, click here and start with the Tic Disorder Cheat Sheet.
Frequently Asked Questions
A tic disorder is a neurological condition involving sudden, repetitive movements (motor tics) or sounds (vocal tics). They range from mild, short-lived tics to chronic conditions such as Tourette’s Syndrome, which includes both motor and vocal tics. Together, these conditions form part of the tic disorder spectrum.
Up to 1 in 5 children experience temporary tics during childhood. Most resolve within months, but chronic tic disorders—including Tourette’s—affect about 0.6% of children. Boys are diagnosed more frequently than girls.
Yes. Research shows that tics can overlap with ASD and ADHD. Around 20–40% of children with autism also experience tics, which differ from repetitive stimming behaviors. ADHD is also frequently reported in children with Tourette’s.
Tics often “wax and wane,” becoming stronger with stress, fatigue, or illness. Environmental exposures, certain foods, and emotional strain may also act as triggers. Keeping a symptom diary can help parents identify patterns.
No single blood test or brain scan confirms tic disorders. Diagnosis is based on clinical history and observation by a healthcare provider. Specialists may use detailed evaluations to rule out other conditions and identify co-occurring challenges.
Tic disorders are influenced by both genetics and environment. A family history raises risk, but factors like infections, pregnancy complications, or environmental stressors may also contribute.
Many children see tics decrease or disappear during adolescence. About 80% experience improvement by late teens, though some continue to have mild tics into adulthood.
Treatment depends on severity. Mild tics may need no intervention, while more disruptive cases can benefit from behavioral therapy (such as CBIT), medication, and lifestyle adjustments. Education and support are key.
Tics are involuntary and often follow a strong premonitory urge, while stimming is intentional and helps regulate emotions or sensory input. Recognizing the difference ensures proper diagnosis and management.
Parents should consult a clinician if tics last longer than a year, involve both motor and vocal tics, or interfere with school, sleep, or social life. Early evaluation helps with accurate diagnosis and effective support
References:
Anderson, E. W., Valuck, R. J., Harris, M. A., Pettit, A., Williams, A., & Simonetti, J. A. (2019). General health and life satisfaction in children with chronic illness. Pediatrics, 143(6), e20182988. https://doi.org/10.1542/peds.2018-2988 https://pmc.ncbi.nlm.nih.gov/articles/PMC6564050/
Hirschtritt, M. E., Darrow, S. M., Illmann, C., Osiecki, L., Grados, M., Sandor, P., Dion, Y., King, R. A., Pauls, D. L., Budman, C. L., Cath, D. C., Greenberg, E., Lyon, G. J., Yu, D., McGrath, C. L., McMahon, W. M., Lee, P. C., Delucchi, K. L., Scharf, J. M., & Mathews, C. A. (2022). Co-occurrence of tic disorders and attention-deficit/hyperactivity disorder. Frontiers in Psychiatry, 13, 956715. https://doi.org/10.3389/fpsyt.2022.956715 https://pmc.ncbi.nlm.nih.gov/articles/PMC9687745/
Moufarrej, Y. E., & Bertolin, J. M. (2024). Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK607260/
Harding, C. F., Pytte, C. L., Page, K. G., Ryberg, K. J., Normand, E., Remigio, G. J., Deiss, T. J., Barry, D., Lane, P. E., Roberts, K. B., Kerut, E. K., Isack, N. R., Rodriguez, C., Stewart, J. E., Rose, G., Thacker, E. I., Kearns, A., English, D., Weir, C., & Screven, L. (2020). Mold inhalation causes innate immune activation, neural, cognitive and emotional dysfunction. Brain, Behavior, and Immunity, 87, 10–20. https://doi.org/10.1016/j.bbi.2019.11.006 https://pmc.ncbi.nlm.nih.gov/articles/PMC7231651/
Chan, L. S., Cheung, H. M., Tsang, S. M., & Cho, D. H. (2019). The blood levels of trace elements are lower in children with tic disorder: Results from a retrospective study. Frontiers in Neurology, 10, 1324. https://doi.org/10.3389/fneur.2019.01324 https://pmc.ncbi.nlm.nih.gov/articles/PMC6928139/
Conelea, C. A., Frank, M., & Belisle, J. (2022). Why tic severity changes from then to now and from here to there. Behavioural Brain Research, 433, 113978. https://doi.org/10.1016/j.bbr.2022.113978 https://pmc.ncbi.nlm.nih.gov/articles/PMC9570874/
Barnett, J. A., Balez, M. R., & Granitto, M. J. (2019). Gut microbiota and neurological effects of glyphosate. Neurotoxicology, 75, 1–8. https://doi.org/10.1016/j.neuro.2019.08.006 https://pubmed.ncbi.nlm.nih.gov/31442459/